- Reference Number: HEY1134/2024
- Departments: Ophthalmology Department
- Last Updated: 31 January 2024
Introduction
This leaflet has been produced to give you general information about your procedure. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
What is Botulinum toxin?
Botulinum toxin is a drug which causes muscles to relax. It is naturally produced by a bacterium called Clostridium Botulinum. More commonly known by the brand name “Botox®”, it is now manufactured for use as a medical treatment for a number of neuromuscular conditions.
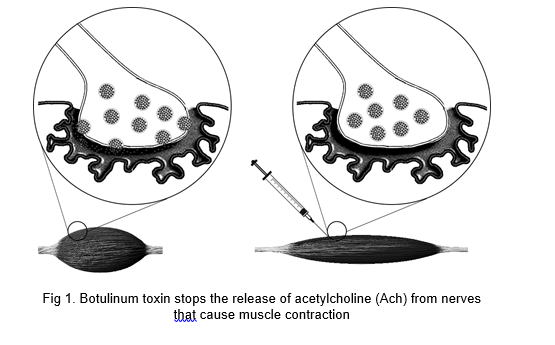
How does Botulinum toxin work?
Nerves connected to muscles cause them to contract by releasing a chemical signal called Acetylcholine. Sometimes this signalling can become overactive, causing involuntary muscular movements such as eyelid spasms and facial tics. In rare cases, prolonged contraction and cramping can result in chronic, debilitating pain. Botulinum toxin temporarily stops nerves from releasing Acetylcholine. Without this neurotransmitter, muscles do not contract and remain in a relaxed state. (Fig 1).
What conditions are Botulinum toxin used to treat?
Botulinum toxin is commonly used to treat the following conditions:
Blepharospasm
Blepharospasm is characterized by abnormal contraction of the muscles around the eye. This can range from a mild eyelid twitch to involuntary blinking or even full closure of the eyelids. It usually affects both eyes, but can sometimes involve just one. The exact cause is unknown, but it is often attributed to a loss of control of the natural blink reflex. Blepharospasm can follow a particular pattern and might be worse at different times of day. It can be triggered by things such as bright light, stress, or fatigue. It often lasts only a few minutes, but in severe cases can last much longer, resulting in difficulty in performing activities of daily life due to difficulty keeping the eyes open consistently.
Hemifacial spasm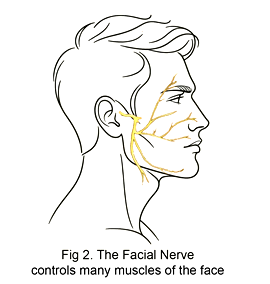
Hemifacial spasm is very similar to blepharospasm. More commonly occurring on just one side of the face, hemifacial spasm involves more muscles than just those around the eye. The cheek and corner of the mouth on the same side contract involuntarily, resulting in what is commonly referred to as a “facial tic.” Hemifacial spasm is better understood than blepharospasm: some patients are found to have a blood vessel that sits in close proximity to the facial nerve (Fig 2), intermittently touching it and causing abnormal activation. Following facial paralysis for other causes (such as Bell’s Palsy), aberrant recovery of the facial nerve can result in paradoxical hyperactivation.
Other eye conditions
Corneal Healing. The cornea is the clear front “window” of the eye. This can be injured by abrasions or ulcers from trauma or infection. If proper healing is at risk due to over-exposure, injecting Botulinum toxin to the upper lid can induce ptosis: drooping of the upper lid over the cornea to protect it from exposure.
Watery Eye. There are many causes of an excessively watery eye. Most of the time, they are caused by poor drainage down the lacrimal apparatus. In some cases, despite adequate patency, it is necessary to “turn off the tap”—that is, to decrease tear production from the lacrimal glands. Injecting Botulinum toxin directly into the gland reduces the amount of tears that it produces constantly, with the goal of reducing the overflow.
Thyroid Eye Disease. Inflammation from thyroid eye disease can cause tissues around the eye to contract, pulling the eyelid upwards. This results in more of the eye’s surface exposed than normal, leading to dryness, redness, and irritation. The eye can also fail to close completely. Botulinum toxin can induce ptosis by relaxing the muscles of the upper lid, allowing them to relax and drop down to cover the eye better.
Are there any other or alternative treatments for blepharospasm and hemifacial spasm?
The first line of treatment for blepharospasm and hemifacial spasms is Botulinum toxin injection. This is usually sufficient for most patients. However, if you wish to try alternative treatments first, or while waiting for your appointment to have the injection, the following may provide some relief:
Avoiding triggers. If you notice spasms in bright light, wear sunglasses before stepping outdoors. Dry eyes can cause reflex blinking, which in turn can trigger involuntary spasms; use lubricant drops to keep your eyes moist. Try and have a good night’s rest if you feel that fatigue triggers your spasms. If you wake up feeling unrested, find it difficult to function without naps, or always feel sleepy during the day, ask your GP to screen you for sleep apnoea.
Patching. Patching the spastic eye may help to shorten the duration of the symptoms by reducing stimuli and protecting it from dryness. Be careful when using an eye patch however: your field of view and depth of perception will be impaired which may result in falls or other accidents.
Compresses. Some patients say that cold compresses help to soothe a spasmic eye. Others find that warm packs relax the area more. Find what works for you.
For severe cases, systemic spasms, and patients refractory to all other forms of treatment, medications prescribed by a Neurologist can help. These however affect the entire body and have their own risks, benefits, and side-effects. Your doctors will advise you if this is the best course of action for you.
How do I prepare for the procedure?
Please read this information leaflet. If you wish, share its contents with others so that they can be as informed and can offer support. There may be things they need to know, especially if they are taking care of you following this procedure.
Points to note:
- The procedure is performed at the Eye Hospital Outpatient Department.
- You should not drive to and from this appointment.
- You should continue to take all your regular medications.
What will happen?
Where to go on arrival
You should report to Reception Desk of the Outpatient Clinic at the Eye Hospital on the Hull Royal Infirmary grounds.
The procedure
After being admitted by Reception and given a wrist band, you will be directed to the waiting area where you are to wait for your name to be called by a member of staff. You will then be directed to the treatment room where a doctor will review your case briefly, discuss the procedure, repeat the risks, benefits, possible complications, side-effects, and manage your expectations. You will be given the opportunity to ask questions. Once you are happy to proceed, you will be asked to sign a consent form, and the treatment will begin.
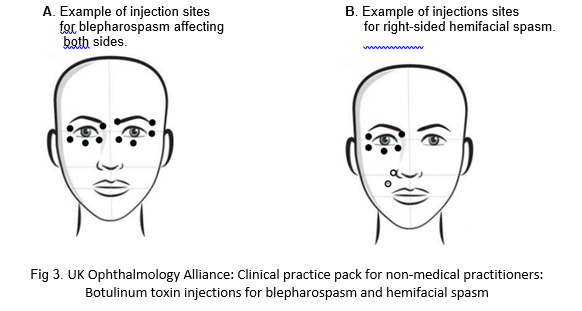
The procedure itself will involve small amounts of Botulinum toxin injected at various sites around the eye and face, wherever required. The exact number varies from person to person, but usually involves between two and six injections per affected are (see Fig 3). The entire process takes only a few minutes. Most patients find the injections to be a little uncomfortable, but manage well.
What should I expect afterwards?
Immediately following the treatment, you may temporarily experience mild pain, redness, or swelling at the injection sites. There may be minimal bleeding. These symptoms are common, and under no circumstances must you apply pressure or rub the injection site. Doing so may cause the toxin to migrate to the surrounding tissues, causing unwanted effects. If you notice some bleeding, take some soft tissue or cotton ball and gently dab the area; the bleeding should stop in a few minutes. Rarely does the pain from Botulinum toxin require an oral pain reliever, but you may if you feel the need to do so.
Noticeable effects of the treatment can be seen as early as three to five days following the injection, with its full effect developing by two weeks. Over this time, you should notice an improvement in your symptoms: decreasing in both frequency and severity.
The effect of Botulinum toxin typically lasts three months, so consistent symptom relief can be achieved with about four to five injections per year. Regular treatment can result in a more prolonged effect, requiring fewer injections over longer periods of time. Very rarely, the opposite can also occur: resistance to the treatment can also develop, leading to more frequent injections in a shorter period of time. Every case is different—even the sites and strength of the treatment administered to you at each visit may vary. One side of your face may respond differently to the other. Many factors interact and play a role in the efficacy of the treatment. Your doctor will be working with you to tailor the appropriate regimen for your symptoms.
Are there any side effects or risks of Botulinum toxin injection?
Localised side-effects
The most common side effects are a direct result of the injection. The following may occur at the injection site:
- Bleeding, bruising, or redness
- Discomfort, pain or tenderness
- A small amount of swelling
- Itchiness
- Tingling or numbness
- Less commonly, infection may occur. This causes significant swelling, pain, and redness at the injection sites. There may also be some discharge.
Sometimes the eye itself can feel slightly irritated, dry, watery or sensitive to light after the procedure. It is uncommon for vision changes to occur following treatment.
Systemic side-effects
Botulinum toxin very rarely causes generalised side-effects. These may include a general feeling of being unwell, having flu-like symptoms, or a headache. These effects usually disappear within a few days.
Risks
As with any treatment, the risk of over or under-correction may occur. These may be the result of insufficient toxin administered (especially if it is your first time, and both you and your doctor are working to tailor your treatment dose), or it spreads to surrounding tissues causing undesirable outcomes.
- Drooping of the upper eyelid. If the treatment is done to lower the upper lid, over-correction may result in complete eye closure.
- Inability to fully close the eyelids. This can lead to dry eye, discomfort, or blurred vision. Very rarely is the cornea severely compromised.
- A change in the position of the lower lid, whether inwards or outwards.
- Double vision, if muscles of eye movement are affected.
- Droop of the corner of the mouth, mimicking the appearance of a stroke.
- Should the medication migrate downwards following injections around the eye, it may also affect other muscles of the face leading to facial paresis. This is a very rare complication of the treatment.
There is no way to reverse the effect of Botulinum toxin. They are, however, temporary and will resolve in three months. While waiting for the toxin to wear off, most symptoms can be managed conservatively. It is important to communicate well with your doctor regarding any post-treatment effects especially during the first few cycles in order to improve the succeeding outcome.
You should seek medical advice urgently if you experience problems with swallowing, speaking, or breathing following any medical treatment.
Is there anyone who should not receive Botulinum injections?
- Anyone with a known allergy to Botulinum toxin.
- You are pregnant or breastfeeding or planning on becoming pregnant.
- Individuals who have an active infection in any of the areas to be injected. This should be treated first and the appointment re-scheduled.
- People with muscular disorders such as myasthenia gravis, as they are at high risk of suffering more dangerous side effects. Always inform your doctor if you have any other known illnesses or are taking any medication.
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the Ophthalmic Department on 01482608788 or Ophthalmology Day Unit (Eye Hospital) on tel: 01482 604385.
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.

