- Reference Number: HEY960/2024
- Departments: Maternity Services
- Last Updated: 30 June 2024
Introduction
This leaflet has been produced to give you general information about Venous Thromboembolism (VTE). It explains what it is, why you are at risk and what you can do to reduce your risk or avoid it. Most of your questions should be answered by this leaflet. It is not intended to replace discussion between you and your midwife or doctor but can act as a starting point for discussion. If after reading it, you have any concerns or require further explanation please discuss this with a member of the healthcare team.
What is venous thromboembolism?
Thrombosis is a clot in a blood vessel (a vein or an artery). The information within the leaflet is about a thrombosis that occurs in a vein (the blood vessels that take blood towards the heart and lungs).
Venous Thromboembolism is a blood clot that can develop deep in the veins of the body. It usually affects the deep veins of the calf, thigh or pelvis and is called a deep vein thrombosis (DVT).
Symptoms of a DVT include:
- A red and hot swollen leg
- Swelling in your entire leg or just part of it
- Pain and/or tenderness – you may only experience this when standing or walking or it may just feel heavy
Seek advice immediately from your doctor or midwife if you notice one or more of these symptoms. During pregnancy, swelling and discomfort in both legs is common and does not always mean there is a problem. Always ask your doctor or midwife if you are concerned.
Why is a DVT serious?
The danger of a DVT is that the clot may break off and travel in the blood stream until it reaches another part of the body such as the lungs and block blood vessels, known as a pulmonary embolus (PE).
The symptoms of a pulmonary embolus may include:
- Sudden unexplained difficulty in breathing
- Tightness in the chest or chest pain
- Coughing up blood (haemoptysis)
- Feeling very unwell or collapsing
Seek help immediately if you experience any of these symptoms.
Although a pulmonary embolus is rare, it can be life threatening. The risk of developing a pulmonary embolus once a DVT has been diagnosed and treated is extremely small.
Why am I at risk?
Pregnant women are ten times more likely to develop venous thrombosis than woman who are the same age and not pregnant. This is mainly because factors in the blood which promote blood clotting increase in pregnancy. Venous thrombosis related to pregnancy can occur at any stage of pregnancy and for six weeks after birth.
Additional risks for developing a venous thrombosis in pregnancy are when you:
- Have had a previous venous thrombosis
- Have a condition called thrombophilia, which makes a blood clot more likely
- Are over 35 years of age
- Are overweight – body mass index (BMI) over 30*
- Have had certain types of fertility treatment
- Are carrying more than one baby (multiple pregnancy)
- Have severe pre-eclampsia
- Have just had a caesarean delivery or a long labour (over 24 hours)
- Are immobile for long periods of time, for example, after an operation or when travelling for four hours or longer
- Are a smoker **
- Are dehydrated e.g. because of severe sickness in pregnancy
- Develop a severe infection e.g. severe kidney or chest infection
- Are admitted into hospital
*For advice on weight management in pregnancy see your Midwife.
**For specialist advice on stopping smoking please ring tel: 0800 915 5959 or visit www.readytostopsmoking.co.uk
What can I do to reduce the risks?
The doctors and midwives will assess what risk factors you may have during your pregnancy and again after the birth of your baby and they may advise one or more of the following:
- Wear anti-embolism stockings. These support stockings help the blood circulation in the legs. Your midwife or doctor will advise you on how long to wear them for.
- Sequential Compression Device. These are inflatable sleeves that are fitted around the calf whilst you are in hospital and immobilised. They inflate at regular intervals and the pressure increases the flow of blood back to the heart.
- Have injections of low molecular weight heparin (an anticoagulant) to ‘thin the blood’. These are usually given as a once daily injection.
- Drink plenty of fluids. You are more likely to develop a DVT if you become dehydrated.
- Remain as mobile as possible. This is very important if you have had a caesarean section. The staff will help you to get out of bed and make sure you have good pain relief.
- Doing this simple exercise to help your blood move around your body:
Lying on your back or sitting
Bend and straighten your ankles quickly. Keep your knees straight during the exercise to stretch your calf muscles. Repeat at regular intervals throughout the day.
How do stockings reduce the risk?
If necessary, you will be measured and fitted for either knee or thigh length white stockings. You should be shown how to fit and wear them. They work by reducing damage to the leg veins that swell when you are not mobile. Small tears to the veins cause activation of the clotting mechanism. They also work by squeezing the blood from the smaller capillaries onto the larger veins in the leg promoting good circulation.
Use and care of the stockings
If stockings are needed they should be worn at all times during your hospital stay and after your discharge. As you should wear the stockings all the time, two pairs will be provided so as to allow you to wash them. When stockings are removed for changing, they should be off for no longer than 30 minutes. The stockings are designed to fit snugly but should not be tight. They should not be creased or rolled down. This will cause an uneven pressure and reduce the blood flow. The stockings can be washed at 40°C, any higher and the stockings may shrink. They can be tumble dried if the machine does not exceed 121°C.
What are anticoagulation injections?
The doctor might consider that you should take an anticoagulation injection of low-molecular-weight heparin which reduces the chance of your blood clotting and stop a DVT from forming. You may hear the injections being referred to as Enoxaparin or Inhixa®, this is the trade name. Heparins are porcine-derived (from pigs) though other drugs are available for those people whose religious views preclude the use of porcine products.
Low-molecular-weight heparin does not cross the placenta to the baby and so is safe to use when you are pregnant. Low molecular weight heparin is also safe to use when breastfeeding.
Whilst you are receiving blood thinning medicines your blood is thinner than normal and so you need to report any unusual symptoms to your doctor, particularly increased bruising, any unusual bleeding or dark ulcers at the injection sites.
Used sharps bins can be returned to hospital (to the area where you were prescribed) or collected by the Council collection service. In order to arrange sharps bin collection by the Council, you will need to ring the following numbers:
- Hull City Council – tel: 01482 300300
- East Riding of Yorkshire Council – tel: 01482 393939
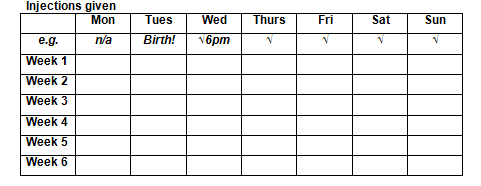
Keep a record
A record like the one below may help you to remember to take your low molecular weight heparin medication.
What should I do if my calf becomes swollen red and painful?
If you experience any of these symptoms, contact your doctor, the Labour Ward on tel: 01482 604390 or the Antenatal Day Unit on tel: 01482 382729 for advice. You should in the meantime leave the stockings off and raise your leg slightly on a footstool.
What should I do if I become breathless or develop chest pains?
Seek help immediately if you experience any of these symptoms either by contacting your doctor or the Labour Ward on tel: 01482 604390. Alternatively, you can attend the Emergency Department.

