- Reference Number: HEY1143-2024
- Departments: Orthopaedics, Physiotherapy
- Last Updated: 24 April 2024
Introduction
This leaflet has been produced to give you general information. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and the healthcare team. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team.
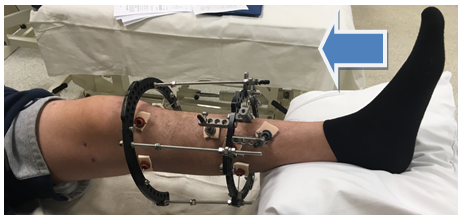
Physiotherapy treatment after application of frame
Information on the application and types of frame can be found in the leaflet ‘Frame Surgery’. This leaflet explains the physiotherapy treatment post application of a frame.
What will happen after my frame surgery?
Post application you will require physiotherapy as an inpatient and then as an outpatient when you are discharged. The physiotherapist will come and assess you on the ward so please ask them if you have any further questions.
Why do I need physiotherapy?
This will aid and speed up you recovery by mobilising the joints and strengthening the muscles in your leg.
Physiotherapy inpatient
External Foot Plate
If your frame does not span into your foot, you will be assessed on the ward by a physiotherapist and a footplate may be made. This is a moulded plastic sole which is attached to your frame to ensure you maintain the best possible foot position and achilles tendon length. The foot plate should be worn during the day 2 hours on / 2 hours off until you are fully mobile. The foot plate should also be worn throughout the night or when you are resting in the day whilst your frame is on your leg unless instructed otherwise. If your foot plate causes foot pain or skin changes please discuss this with your physiotherapist. Please note the foot plate is not designed to be used for weight bearing on.
Walking
Most patients are allowed to walk straight away with a frame on. You will be assessed by the physiotherapy team and provided with appropriate walking aids to ensure you are safe; this may be crutches or a walking frame. Your mobility, confidence and independence will gradually progress. You will only be allowed to be discharged home once the physiotherapy team have assessed you as safe, this may include a stair assessment where necessary.
Exercises
Foot exercises will be carried out to maintain joint movement, if your frame allows. You will also be taught home exercises including elevation (to minimise swelling), ankle and knee movement exercises (to minimise stiffness), and basic strength exercises (to minimise muscle wasting).
Exercises should be performed at regular intervals throughout the day or as pain allows.
Inpatient physiotherapy exercises
1. Elevation
The frame leg should be elevated above the hip with your knee straight when you are at rest. Do not let your knee bend while your leg is elevated. Maximum time 20 minutes. After 20 minutes change the position of your leg to ease the pressure on your heel and prevent the development of a pressure sore.
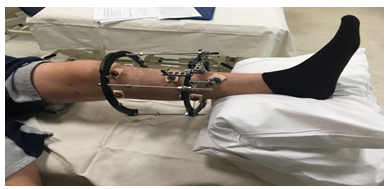
(Photo courtesy of Hull Limb Reconstruction Service)
2. Static quad
Push the back of your knee into the bed and pull your toes up, tightening your thigh muscle. Hold for 10 seconds and repeat 10 times per waking hour.
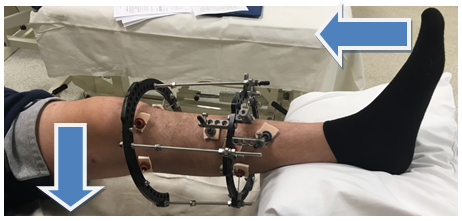
(Photo courtesy of Hull Limb Reconstruction Service)
3. Knee slides
Bend and straighten your knee as much as possible, use your foot to slide along the bed. Repeat 10 times every waking hour.
(Photo courtesy of Hull Limb Reconstruction Service)
4. Achilles stretch
Using a bandage or towel around your foot pull your foot up towards you and hold for 30 seconds at a time. Repeat 10 times every waking hour.
(Photo courtesy of Hull Limb Reconstruction Service)
Physiotherapy outpatient
You will be referred to outpatient physiotherapy by the ward physiotherapists.
If you are local to the area, you will be expected to attend physiotherapy regularly at Hull Royal Infirmary until you are independent and any adjustments to your frame have been completed. Patients who live out of area will have physiotherapy closer to home. During your physiotherapy sessions you will complete an individualised exercise program.
The frequency of your physiotherapy sessions will be assessed by your treating physiotherapist and modified according to your individual needs.
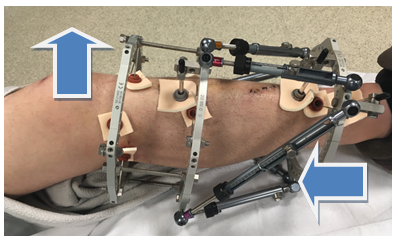
The main aims of physiotherapy are:
- Maintenance of knee, ankle and foot movement, and achilles length
- Progression of weight bearing, walking, and functional ability
- Strengthening of the muscles around the hip, knee, and ankle

(Photo courtesy of Hull Limb Reconstruction Service)
Lifestyle choices
There are many factors that can influence the healing process, listed below are some of the factors that you can directly influence:
- Smoking: Research has proven that smoking can significantly delay the bone healing process. It is therefore vital that you quit smoking in order to achieve optimum healing and to prevent delayed or non-union (healing). Smoking cessation is available you can self refer, ask the staff on the ward or visit your doctor. Please note passive smoking is also detrimental to bone healing and family should therefore be encouraged to stop smoking too. NHS Smoking cessation line: tel: 0300 123 1044
- Diet: A good balanced diet will promote optimum bone healing, foods such as oily fish, green vegetables and lentils are recommended. Research has shown that carbonated drinks (pop and energy drinks) can delay bone healing as they deplete the body of calcium. Alcohol consumption has also been shown to be detrimental to the bone healing process.
- Work: Sedentary (sitting) workers may be able to return to work after six weeks although this will need to be discussed at your outpatient clinic appointment. More active jobs will require discussion with your consultant and you may need to be assessed by your employers own occupational health team.
- Emotional well-being: It is not uncommon to experience low mood or depression following the application of circular frame. Changes in mood can effect motivation and compliance which in turn can have an effect on healing and progression. If you are feeling low in mood or are concerned about depression see your doctor who can prescribe medication and refer you to counselling services if necessary.
- Driving: Once you can safely control your vehicle and perform an emergency stop without hesitation, you can return to driving. Some patients do find their leg does not fit in the foot well of their car. You should inform your insurance company and your DVLA that your have had this surgery to ensure it does not affect your policy.
Frame duration
How long your frame is on for will primarily be determined by how severe your fracture or deformity correction is. Compliance with rehabilitation and maintaining a healthy lifestyle and diet also have a bearing on timescales of treatment.
You will have regular X-rays whilst your frame is on, to monitor bone-healing. Once your consultant is satisfied with your bone healing staged frame removal can begin; this will involve “reloading” of the bone by way of removing the struts in the clinic setting, followed by removal of the rings 2 to 4 weeks later in clinic. If you decide to have the frame to be removed under anaesthetic you may wait for a slot to become available for this to be done.
In the event of the “reloading” causing pain at your fracture or correction site, you will be reviewed in clinic and the struts may be replaced for further period of time.
Once your frame is fully removed you will continue to be monitored by the physiotherapy team where your goals will be reviewed and rehabilitation will continue until agreed goals have been met or physiotherapy is no longer effective.
Further advice
Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the team via the Fracture Clinic or other specialist on tel: 01482 674378
The answer machine is accessed 7 days a week in working hours, this is the best way to contact the team. If you leave your contact details someone will contact you for more information and advice. They will put you in contact with a member of the frame team if needed.
Other useful numbers:
Physiotherapy Department – tel: 01482 674880
Clinical Lead Nurse – tel: 01482 674942, Monday to Friday 8:00 am to 4:00 pm. Out of hours and weekends, tel: 01482 674368
Clinical Lead Physiotherapist: tel: 01482 674942
General Advice and Consent
Most of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion with the healthcare team.
Consent to treatment
Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information.
The information you receive should be about your condition, the alternatives available to you, and whether it carries risks as well as the benefits. What is important is that your consent is genuine or valid. That means:
- you must be able to give your consent
- you must be given enough information to enable you to make a decision
- you must be acting under your own free will and not under the strong influence of another person
Information about you
We collect and use your information to provide you with care and treatment. As part of your care, information about you will be shared between members of a healthcare team, some of whom you may not meet. Your information may also be used to help train staff, to check the quality of our care, to manage and plan the health service, and to help with research. Wherever possible we use anonymous data.
We may pass on relevant information to other health organisations that provide you with care. All information is treated as strictly confidential and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you.
Under the General Data Protection Regulation and the Data Protection Act 2018 we are responsible for maintaining the confidentiality of any information we hold about you. For further information visit the following page: Confidential Information about You.
If you or your carer needs information about your health and wellbeing and about your care and treatment in a different format, such as large print, braille or audio, due to disability, impairment or sensory loss, please advise a member of staff and this can be arranged.